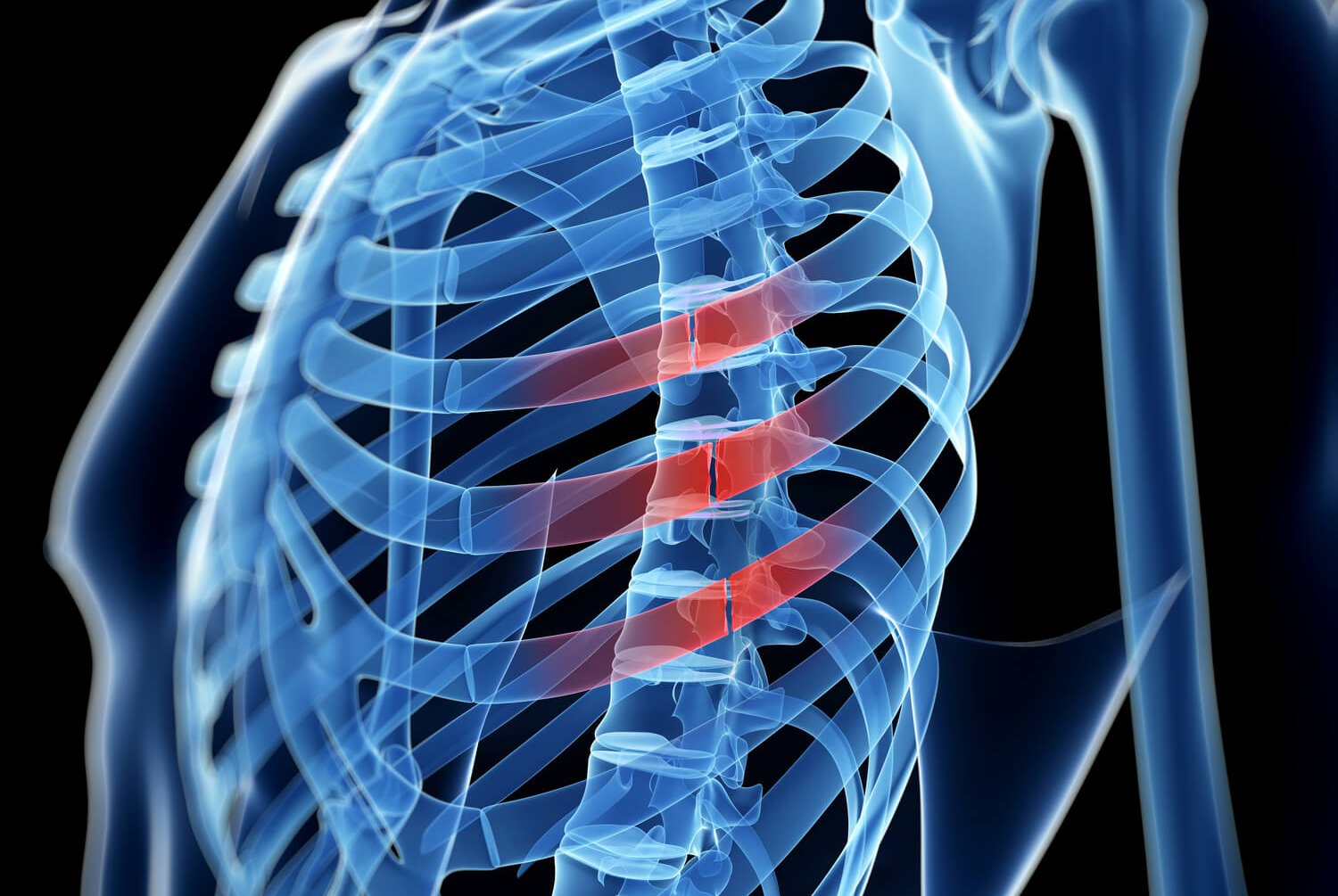
Back Pain
Back pain effects more than 85% of all Americans during their lifetime. It can have many causes such disc, joint, ligament/bone or muscular pathology. Acute pain (less than six weeks onset) is usually self-limited. Immediate medical attention should be sought when weakness, loss sensation, or bladder/bowel changes accompany the pain. Tumors and malignant causes of pain are rare, occurring in less than 1% of those people suffering from back pain. However, this should be further looked at if neurologic changes occur and the pain doesn’t resolve with treatments. While acute pain is usually recognized as only lasting approximately 6 weeks, chronic pain is generally termed after 12 weeks. Bed rest is not advised, nor is the use of a lumbar support belt for more than two weeks. Most sources of pain respond to conservative treatments, which may include physical therapy, anti-inflammatory medications, topical pain relievers and cortisone injections. Unfortunately, there is a subset of people whose pain is so severe that activities or work are extremely limited during the first six weeks. Or, the pain extends beyond six weeks and approaches the chronic stages of a condition. For these groups of patients, many will respond to interventional pain procedures.
There is no blood test for pain. The diagnosis and treatment require the performance of a careful history and physical exam, along with the use of radiographs (xray, MRI, CT). EMG and nerve conduction studies may also be indicated.
Common causes of back pain include: lumbar disc bulge, lumbar disc herniation, degenerative disc disease, joint inflammation (both facet and sacroiliac), sciatica (pinched nerve), fractures of vertebrae, lumbar spinal stenosis, and prior back surgery (also known as post laminectomy syndrome.
Treatments: Many patients will not respond to the conservative treatments as described above. For those non-responders, interventional pain procedures may be indicated. These interventional treatments, determined by the condition, may include: epidurals, facet blocks, sacroiliac joint injections, MILD procedure, radiofrequency lesioning, neuroplasty/lysis of adhesions, kyphoplasty, and spinal cord stimulator.